Howie's column is powered by Lyric Kitchen · Bar
In the offices of Essentia Health, the phrase “honoring Tribal sovereignty” isn’t carved on a wall — it’s built into the work.
It means Indigenous Nations are treated as co-creators of the rural health system itself, shaping the care that reaches their own people.
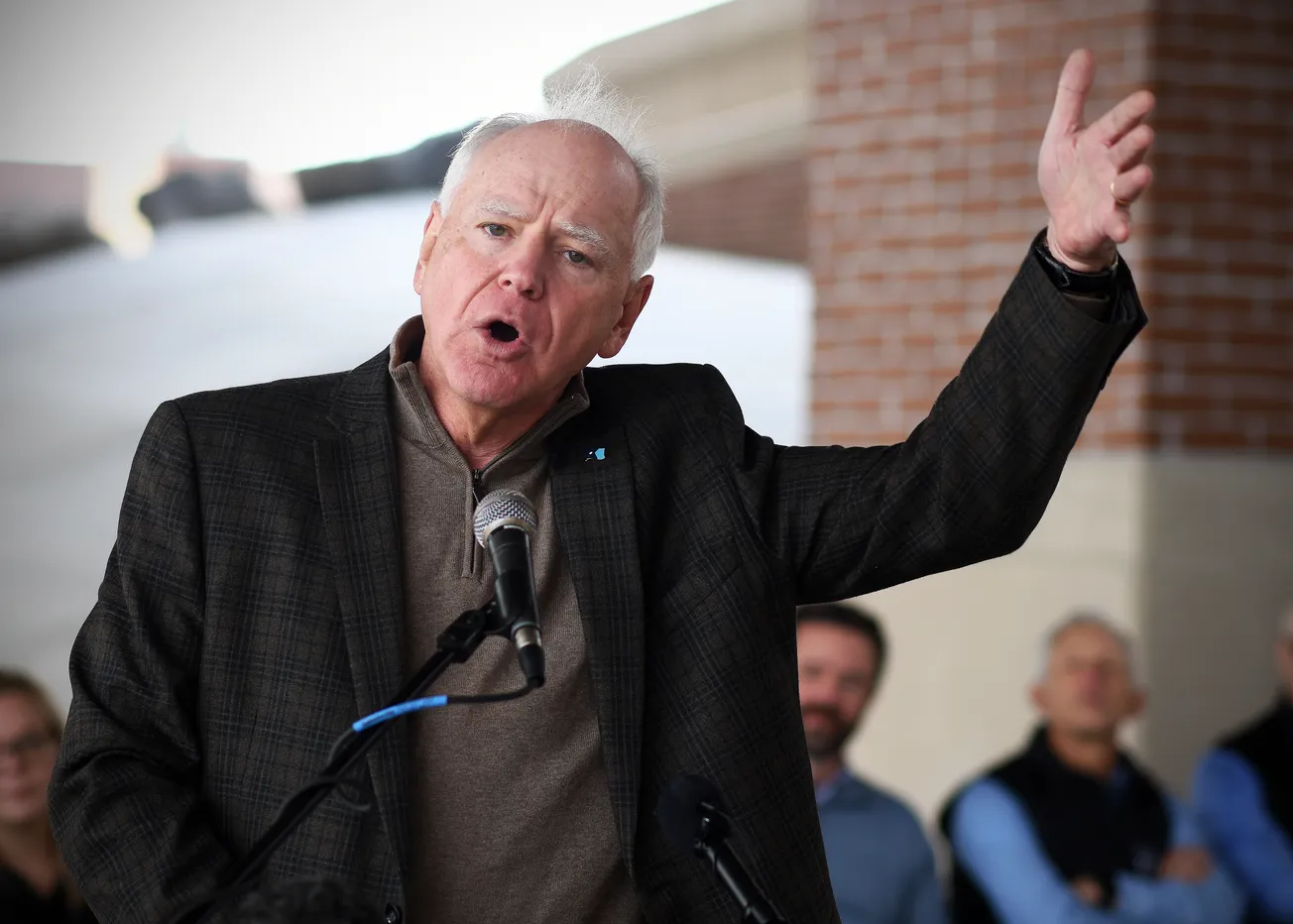
That philosophy, voiced and lived by Samuel Moose, Essentia’s director of Tribal Government Relations, has quietly redrawn the map of medicine in northern Minnesota.
Drive an hour north of Duluth and the picture of “rural Minnesota” changes. The familiar postcard of white farmsteads and fishing shacks gives way to Ojibwe lands, Somali groceries, Hmong farms, and towns where poverty and resilience share the same main street.
Rural Minnesota is no longer a single color, if it ever was — and Essentia Health has become the national example of what happens when a system decides to treat that truth as data instead of discomfort.

When Essentia screened 144,000 patients for social needs, the results forced a reckoning. Food insecurity affected 22 percent of American Indian and Alaska Native patients, 17 percent of Black patients, and 7 percent of white patients.
Transportation and financial barriers followed the same curve. The numbers revealed what many rural clinicians already knew in their bones: geography hides inequity, but it doesn’t erase it.
Under CEO Dr. David Herman, Essentia built a response equal to the problem. Every patient’s social needs now live inside the electronic medical record. When hunger or lack of transport blocks care, an automatic referral goes to a partner — a Tribal council, food bank, or public-health agency — and staff can track whether help actually arrived.
It’s equity turned into infrastructure.
Moose calls it shared responsibility. His words echo through the organization: that sovereignty isn’t a courtesy extended to Native Nations, it’s the framework that makes health care honest. The partnership model has become Essentia’s signature — and Minnesota’s new export to the nation.

"In rural communities, where disparities are deep and resources are often scarce, collaboration with Tribal governments is essential to building resilient, responsive, and equitable care models," Moose said. "Essentia is proud to stand with, and build systems alongside, the Indigenous communities we're privileged to serve.”
The results speak for themselves. By publishing outcomes through Minnesota Community Measurement, Essentia not only surpassed the statewide average on 13 of 21 quality metrics, it changed the conversation about what rural systems can achieve. Transparency became a competitive advantage. Accountability became culture.
On the ground, the data turns into lives. In Fond du Lac, prenatal appointments now line up with childcare and transportation schedules. In Bemidji, the mother who once missed half her visits keeps every one. In Moorhead, Somali elders finally finish telehealth sessions because broadband upgrades stick. Each story is a small victory, but together they redefine what rural health looks like.
National policy is catching up. Congress has authorized a $50 billion Rural Health Transformation Program requiring states to prove how they’ll reach neglected populations. The Save America’s Rural Hospitals Act and the Health Equity and Accountability Act follow the same path, tying federal dollars to measurable progress.
Minnesota is already moving faster. New legislation rewrites reimbursement formulas to account for transportation, broadband, and cultural access. The state’s definition of “rural health” now stretches beyond geography — it includes who is being heard.

Those laws could have been written in Duluth. Essentia’s model is the template: measure need honestly, publish the truth, share power with those most affected, and keep score.
Trust, Moose reminds his colleagues, can’t be legislated — but it can be earned. Essentia earns it in data and in silence, over kitchen-table meetings and hospital hallways where Tribal leaders sit as equals. What once passed as “outreach” has evolved into co-creation. The difference is more than semantics; it’s survival.
Every partnership is another act of repair. Tribal governments help design maternal-health programs. Community food banks appear in digital referral menus. Students from Indigenous communities train inside Essentia clinics. Each connection blurs the old line between patient and partner.
Compassion alone never changed a system. Measurement did. Herman’s genius has been combining both — proving that empathy can be tracked, audited, and improved like any medical metric. It’s the science of respect.
Federal officials now quote the same language Moose uses — co-creation, partnership, trust. Academic centers are calling Duluth for guidance. The national dialogue has shifted from saving rural hospitals to transforming rural health.
And yet, the stakes remain fragile.

Reimbursement cuts still hover. Staffing shortages threaten to undo progress. But the blueprint stands. Shared power — data in one hand, dignity in the other — is the only sustainable cure.
Shared power looks like a Tribal council drafting clinic policy. It looks like a pastor running a food shelf linked directly to a doctor’s tablet. It looks like a mother arriving for prenatal care because someone finally fixed the transportation barrier instead of scolding her for missing an appointment.
That is what rural transformation looks like. Slow, imperfect, relentless — and real.
On the cold shore of Lake Superior, the country’s most progressive health-equity movement didn’t come from a think tank or a grant. It came from a partnership between a health system willing to publish its own flaws and a Tribal leader who reminded it what sovereignty really means.
The color of rural health is no longer a blank canvas of assumption. It’s a spectrum — Native, Black, brown, white — bound by geography and shared hope. It’s proof that data and dignity can share the same chart, that sovereignty and science can stand side by side.
And it started here, in Duluth, where Moose’s quiet conviction and Herman’s data merged into something larger: a promise kept.
Howie Hanson has reported on health care, politics and regional economics in Minnesota for more than five decades. His work focuses on the intersection of policy and people — where hospital corridors, legislative chambers, and small-town streets all tell the same story.
Editor's Note: Minnesota’s Rural Health Reckoning is an editorial journey through the state of rural health care in Minnesota, featuring one column each day for 13 days.
It looks beyond the headlines and into the exam rooms, the nurse stations, the broadband gaps and backroads where small-town medicine is quietly being rebuilt. Each installment examines one piece of the transformation — from how hospitals survive when the math stops working to how doctors, nurses, and patients are rewriting the rules of care from the inside out.
The story begins in Duluth, where Essentia Health has spent the past decade turning words like “value-based care” into something that actually lives in rural communities. But this isn’t just a health system’s story — it’s ours. What happens to medicine in Minnesota’s small towns will define who we are, how we age, and whether we can still look after one another when it matters most.
No organization sponsored this reporting. No PR firm pitched it. It’s one veteran columnist watching Minnesota’s health-care revolution unfold from the inside out — and trying to make sense of what it means for all of us.