Howie's column is powered by Lyric Kitchen · Bar
You can tell the health of a town by the glow of its pharmacy window. When it goes dark, the community doesn’t just lose a business — it loses the nerve ending that connects it to modern medicine.
The prescription refills, the insulin, the trust across the counter — they all depend on a federal program so obscure most Americans have never heard of it. It’s called 340B. And right now, it’s dying the way rural hospitals die — quietly, through attrition, litigation, and indifference.
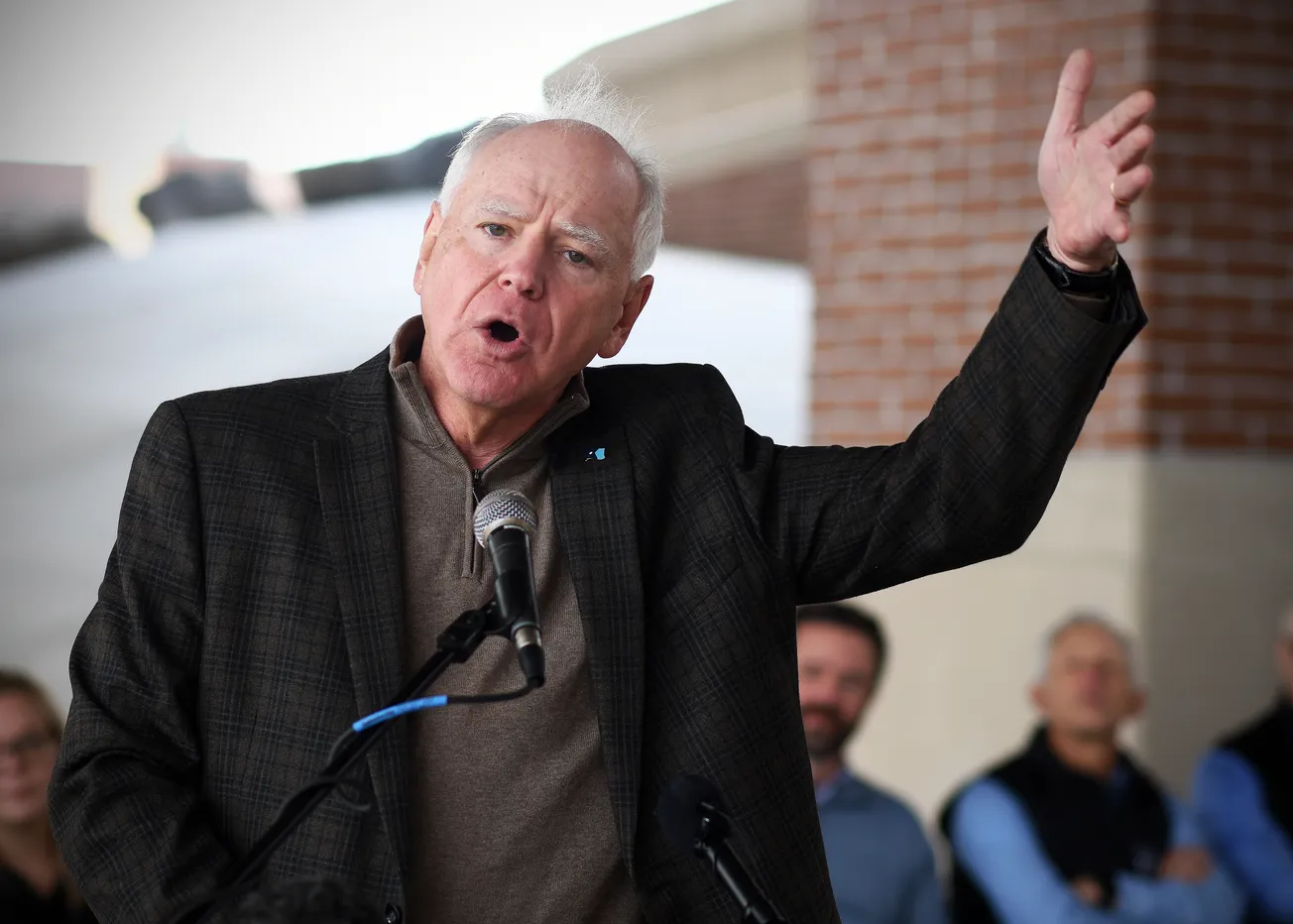
No one has explained this slow suffocation more clearly than Dr. David Herman, the physician-executive who runs Essentia Health in Minnesota, Wisconsin and North Dakota.
Herman didn’t ask to become a national voice. He is a surgeon by training, built for precision and calm, not politics. But when pharmaceutical giants began cutting off discounted drug access to the hospitals that treat the poorest and most isolated patients in the country, he decided silence was no longer neutral.
“The 340B Prescription Drug Discount Program helps rural hospitals stretch limited federal resources and is used to support health services and programs throughout our communities,” he told senators. “Protecting this program is crucial.”

He’s right. The program allows qualifying hospitals to buy outpatient drugs 20 to 50 percent below market price and reinvest the savings in everything the market ignores — behavioral health, oncology outreach, and the small-town pharmacies that act as informal emergency rooms.
In Eveleth or Grand Marais, those pennies per pill become chemotherapy in January, insulin in March, or gas money for a patient driving 80 miles for a mammogram.
The economics are straightforward. The morality is not. Pharmaceutical companies now argue that 340B costs them too much, and they have begun dictating where discounted drugs can be dispensed. They call it reform.
Dr. Herman calls it what it is: “unlawful restrictions that negatively impact hospitals and the ability to acquire prescription drugs under the program.”
A pharmacist in Two Harbors told me half her customers couldn’t afford insulin without 340B. She keeps their names on handwritten cards behind the counter, cross-referenced with the dates they last filled their prescriptions.
“Take away 340B,” she said, “and I can tell you how many funerals I’ll attend next winter.”

Congress has finally noticed. In March 2024, lawmakers introduced the 340B PATIENTS Act, requiring drug manufacturers to honor discounts even when small hospitals partner with community or specialty pharmacies.
The PROTECT 340B Act soon followed, forbidding pharmacy-benefit managers from reimbursing 340B hospitals at lower rates simply because they serve poor people.
For the first time in years, there’s movement in Washington that could actually save rural healthcare instead of just studying it. Still, the industry lobby is stronger, better funded, and less patient.
The lawsuits keep coming — Eli Lilly, Johnson & Johnson, Merck — each arguing that the federal government has overstepped. Courts in the Eighth Circuit have sided with states like Arkansas, which passed laws defending hospital contract pharmacies. Other states are racing to copy the model before Congress can even agree on definitions.
All the while, the math gets worse. Nationally, hospitals in the 340B program purchased about $66 billion in outpatient drugs last year, receiving roughly $46 billion in manufacturer discounts. To a Wall Street balance sheet, that’s a rounding error.

To a critical-access hospital in Hibbing or Ely, it’s the oxygen line. Pull it and the system flatlines.
Dr. Herman has become the calm in the middle of this storm — a measured advocate who can walk senators through the compliance forms, the pharmacy audits, the real-world consequences. He doesn’t raise his voice. He doesn’t need to.
“These savings help provide essential services to our communities,” he said. “Protecting it is vital for rural health.”
He knows what’s at stake because he’s seen what happens when a hospital closes. The economy buckles. The school loses a nurse. The volunteer fire department becomes the ambulance service. People delay care until it’s too late, and then politicians hold hearings about why people die sooner in rural America.
What makes 340B remarkable is its efficiency. It costs taxpayers nothing. It takes from the most profitable sector of American capitalism and redirects a sliver of that margin to the most fragile. It’s not charity. It’s equilibrium. And it works.

The fight now is over who controls that balance — doctors and patients, or corporations and algorithms. When Dr. Herman sits before a Senate panel, he’s not defending a program. He’s defending the idea that the health of a nation should be measured not by shareholder earnings, but by whether a nurse in Moose Lake can still fill a patient’s prescription at closing time.
He didn’t go to Washington to pick a fight. He went to explain reality. The 340B program works. It’s one of the few federal ideas that still does.
If Congress listens, the windows will stay lit — faint, warm, and alive, the last light between survival and surrender in the towns most Americans will never visit but still depend on to remind them what fairness looks like.
Howie Hanson has reported on health care, politics and regional economics in Minnesota for more than five decades. His work focuses on the intersection of policy and people — where hospital corridors, legislative chambers, and small-town streets all tell the same story.
Minnesota’s Rural Health Reckoning — A Special Report by Howie
How Minnesota is quietly rewriting the rules of rural health care
Dr. David Herman is trying to rebuild a model that never fully existed — one that honors the spirit of small-town care while surviving the economics of modern medicine.
Examines the rural-urban digital divide through the lens of telehealth. Nearly 20 percent of rural Minnesotans still lack reliable broadband — meaning no video visits, no remote monitoring, no equity. Puts faces to the stats: seniors, veterans, parents juggling three jobs.
The 96-Hour Rule That’s Breaking Rural Hospitals
Herman’s call to scrap the federal 96-hour limit on Critical Access Hospital stays. Show what happens when a pneumonia patient is too sick to discharge but too “long” to bill.
The 340B Lifeline Under Attack
Big Pharma’s assault on the 340B discount program threatens small-town hospitals. Translated: a few cents in Washington could close pharmacies in Grand Marais or Park Rapids.
From Fee for Service to Fee for Results (Friday)
A plain-spoken explainer of the national shift to value-based care — with Duluth as Exhibit A. Herman’s testimony and local clinicians.
Food, Heat, and Hope: The Social Side of Medicine (Saturday)
Essentia’s 144,000-patient social-needs screening exposes hidden poverty in the Northland. When 14 percent of patients report food, housing, or transport insecurity, the clinic becomes a front line against generational hardship.
The Color of Rural Health (Sunday)
Focus on racial disparities in northern clinics: why 22 percent of Native patients report food insecurity vs. 7 percent of whites. Brings in tribal health directors and shows how Herman’s data demands new partnerships between hospitals and reservations.
The Next Great Minnesota Export: Rural Health Innovation (Monday)
Frames Duluth as a policy lab. How Essentia’s success in value-based care could serve as a model for the Dakotas, Iowa, and Wisconsin — the same way Mayo exported tele-stroke.

When Hospitals Become Economic Engines (Tuesday)
Follows the dollars: rural hospitals like Deer River or Ashland are now the largest employers for 50 miles. Details Herman’s $430 million in community investment and how “healthcare capital” props up Main Street economies.
The Doctor Will Text You Now (Wednesday)
Profiles Essentia’s embedded tech — patient portals, nurse hotlines, “Virtual Visits on Demand.” Asks whether tech can rebuild trust in small-town medicine or just widen the gap between those online and those left out.
Un-Burdening the Healers (Thursday)
Probes clinician burnout and the quiet hope behind Herman’s claim that value-based care restores purpose. Pairs physician interviews with workforce data — the new rural exodus of nurses, the pipeline from St. Scholastica and Itasca CC.
Policy from the North: How Duluth Is Whispering in Congress’s Ear (Next Friday, October 31)
A reporter’s take on Herman’s Washington moment. Charts how Duluth’s CEO is lobbying for permanent telehealth, ACO bonuses, and parity between Medicare Advantage and alternative payment models — small-town voices shaping national reform.