About This Series
Column 2 continues an editorial journey through the state of rural health care in Minnesota. The 13-part series is called “Minnesota’s Rural Health Reckoning.” It looks beyond the headlines and into the exam rooms, the nurse stations, the broadband gaps and backroads where small-town medicine is quietly being rebuilt. Each installment examines one piece of the transformation — from how hospitals survive when the math stops working to how doctors, nurses, and patients are rewriting the rules of care from the inside out.
Essentia Health has spent the past decade turning words like “value-based care” into something that actually lives in rural communities. But this isn’t just a health system’s story — it’s ours. What happens to medicine in Minnesota’s small towns will define who we are, how we age, and whether we can still look after one another when it matters most.
No organization sponsored this reporting. No PR firm pitched it. It’s one veteran columnist watching Minnesota’s health-care revolution unfold from the inside out — and trying to make sense of what it means for all of us.

Howie's column is powered by Lyric Kitchen · Bar
In northern Minnesota, “high-speed” internet can still mean a spool of wire dangling off a light pole. For many families, a Zoom doctor visit still drops like a cell call in a thunderstorm. That digital static is no longer an inconvenience — it’s a public-health crisis with a body count.
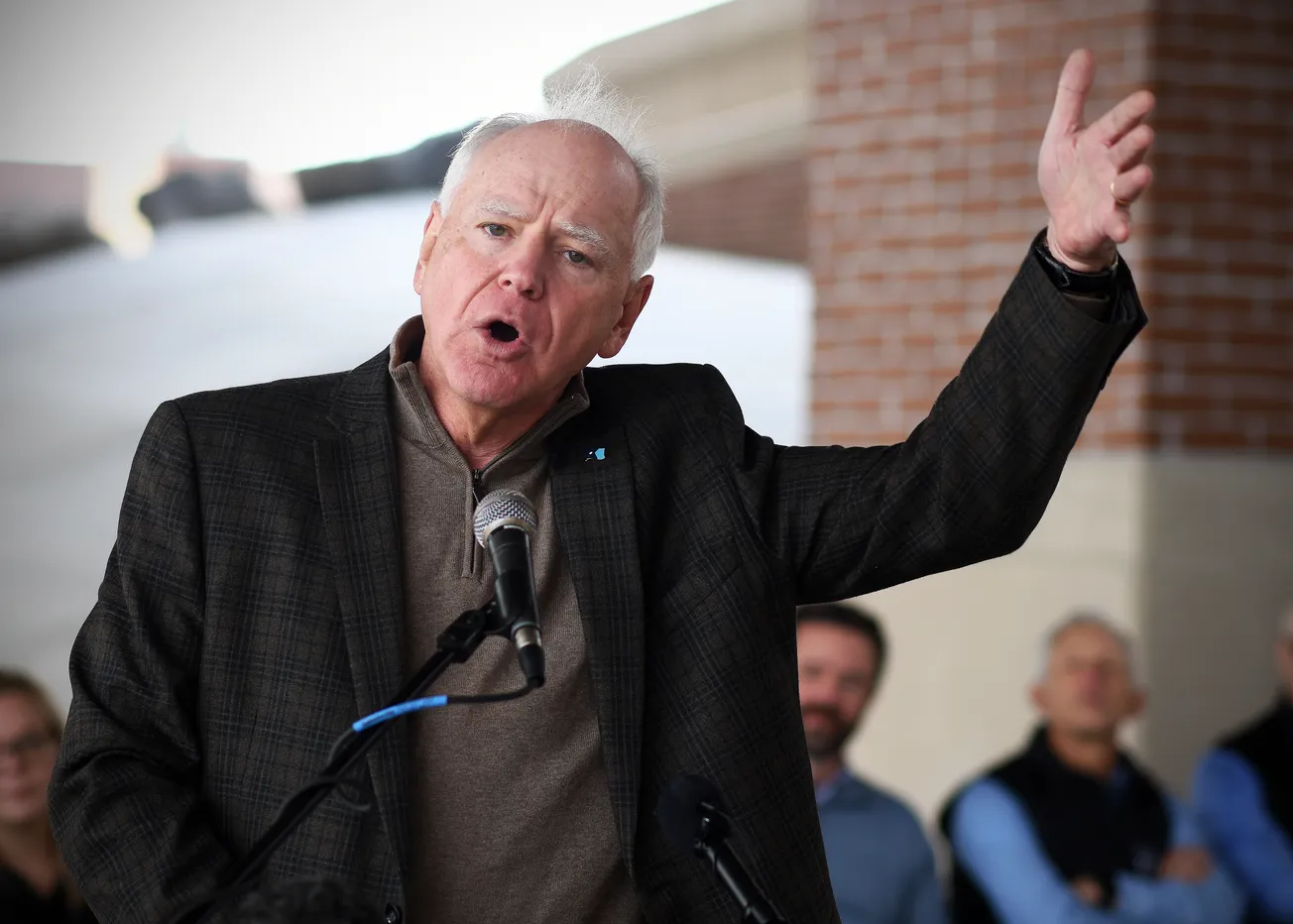
Essentia Health president and CEO Dr. David Herman told the U.S. Senate what rural Minnesotans already know: telehealth is only as good as the connection.
“Over 25 percent in Wisconsin and almost 20 percent in rural Minnesota lack reliable broadband internet for use in video visits,” he said. “That’s a barrier to accessing virtual services that were critical during the pandemic.”
The numbers translate to roughly one in five households where a doctor’s face still freezes mid-sentence — a momentary glitch that, for some, can delay prescriptions, diagnoses, or even survival.

Telehealth was supposed to erase distance. Instead, it has exposed who the system forgot. When the COVID lockdowns hit, Essentia Health rolled out Virtual Visits on Demand and a 24-hour nurse line tied directly into its electronic health-record network. Urban patients adapted overnight. But out on the Range, where DSL lines run through pine and ice, families ended up driving to library parking lots or gas stations just to borrow Wi-Fi for a ten-minute consult.
Herman sees broadband as medical infrastructure, not luxury.
“Patients in rural areas must travel greater distances to access inpatient services,” he told lawmakers. “When telehealth is not an option, those miles become barriers to care.”
For one diabetic patient in Aitkin County, those barriers turned literal. After losing connection three times during an insulin check, she finally gave up, warmed her car, and drove 97 miles to Duluth through a snow advisory. That is what inequality looks like in 2025 — not a policy paper, but a windshield.

What has emerged across rural America is a new kind of emergency room — invisible, digital, and often silent. In cities, fiber-optic cables hum with data. In the country, they simply stop. Entire counties remain uncovered by the modern health grid, their residents relying on the same copper lines that carried party-line calls half a century ago. It is one of the last frontiers of inequality in American medicine, and its boundaries are drawn not by wealth or will, but by signal strength.
The gap isn’t just technological. It’s moral. Without reliable internet, patients can’t refill prescriptions, see a therapist, or upload heart-monitor data. Clinics can’t track blood pressure remotely or conduct follow-ups for COVID-long-haulers.
For rural elderly who gave up driving, digital care is the only care. For veterans or tribal members living on federal lands, the lack of connectivity compounds decades of underinvestment.
Herman argues that Congress should treat broadband the same way it treats roads and bridges.
“If rural America can’t connect, rural America can’t heal,” he said.

Essentia’s strategy has been to focus less on billing codes and more on outcomes — a point Herman stresses in nearly every conversation.
“Our clinicians still need to make sure they are entering the correct code for the service,” he said in a recent note, “yet the focus of the system of care is health outcomes rather than codes generated. We have shown that when you build the system of care to support health, health improves, costs decrease, and rural care can be sustained, at least so far.”
That philosophy defines the quiet revolution now underway in rural medicine. For decades, hospital systems were measured by how efficiently they coded — the bureaucratic shorthand that converts every cough and suture into a billable transaction.
Herman’s view flips that equation. The metric that matters, he argues, isn’t paperwork precision but patient progress. A health-care economy obsessed with codes generates data; a system built around outcomes generates trust.

This is where broadband and philosophy intersect. A doctor’s ability to see a patient online is useless if the technology ends at the township border — and the best intentions collapse if the reimbursement model still rewards volume instead of value.
Herman’s approach links the two: infrastructure plus integrity. Build the digital bridge, then use it to deliver care that counts.
Still, the threats to that fragile system are mounting. Herman warns that “our region will be disproportionately affected by the changes in OB3, particularly the loss of subsidies and tax credits for purchasing insurance on the exchange.”
Those subsidies were lifelines for farmers, small-business owners, and independent contractors — the backbone of rural economies that rarely offer employer-based coverage. Their disappearance would be felt immediately in waiting rooms and on monthly statements.
The OB3 shift sounds like policy jargon, but its effect is intimate. Fewer subsidies mean fewer insured patients, fewer appointments, and more delayed diagnoses. For small rural hospitals already balancing on tight margins, it could mean the difference between staying open and turning off the lights.
Broadband won’t matter much if the clinics at the other end of the line can no longer afford to exist.
Broadband may be the headline issue, but insurance stability is its quiet twin. Without predictable reimbursement and affordable coverage, the gains from telehealth evaporate. Clinics can’t invest in technology when they don’t know if next year’s patients can even afford to log in.
If Washington wants proof that digital medicine works, Herman can provide it: lower readmissions, higher patient satisfaction, and fewer miles driven by ambulances that were never needed.
Those metrics are hard to ignore — and even harder to fund if the broadband lines stop short of the county line. Essentia has lobbied for permanent telehealth reimbursements and flexible licensing across state lines, so a patient in Cloquet can consult a specialist in Fargo without paperwork gymnastics. But none of it matters without bandwidth.

What’s at stake is not just medical access but the survival of the rural-care model itself. In places like Hibbing, Aitkin, or Grand Rapids, every dropped signal becomes another reminder of distance — between urban and rural, insured and uninsured, connected and forgotten.
Telehealth, Herman insists, is not a shortcut but a lifeline. The proof is already visible: fewer hospitalizations, lower costs, and improved patient outcomes. What’s missing is the will — and the infrastructure — to finish the job.
“Broadband is the new stethoscope,” Herman said.
It’s hard to argue with a doctor who’s been listening to static for twenty years.

Minnesota’s Rural Health Reckoning — A Special Report by Howie
How Minnesota is quietly rewriting the rules of rural health care
Dr. David Herman is trying to rebuild a model that never fully existed — one that honors the spirit of small-town care while surviving the economics of modern medicine.
Examines the rural-urban digital divide through the lens of telehealth. Nearly 20 percent of rural Minnesotans still lack reliable broadband — meaning no video visits, no remote monitoring, no equity. Puts faces to the stats: seniors, veterans, parents juggling three jobs.
The 96-Hour Rule That’s Breaking Rural Hospitals
Herman’s call to scrap the federal 96-hour limit on Critical Access Hospital stays. Show what happens when a pneumonia patient is too sick to discharge but too “long” to bill.
“The 340B Lifeline Under Attack
Big Pharma’s assault on the 340B discount program threatens small-town hospitals. Translated: a few cents in Washington could close pharmacies in Grand Marais or Park Rapids.
From Fee for Service to Fee for Results
A plain-spoken explainer of the national shift to value-based care — with Duluth as Exhibit A. Herman’s testimony and local clinicians.
Food, Heat, and Hope: The Social Side of Medicine
Essentia’s 144,000-patient social-needs screening exposes hidden poverty in the Northland. When 14 percent of patients report food, housing, or transport insecurity, the clinic becomes a front line against generational hardship.
The Color of Rural Health
Focus on racial disparities in northern clinics: why 22 percent of Native patients report food insecurity vs. 7 percent of whites. Brings in tribal health directors and shows how Herman’s data demands new partnerships between hospitals and reservations.
The Next Great Minnesota Export: Rural Health Innovation
Frames Duluth as a policy lab. How Essentia’s success in value-based care could serve as a model for the Dakotas, Iowa, and Wisconsin — the same way Mayo exported tele-stroke.
When Hospitals Become Economic Engines
Follows the dollars: rural hospitals like Deer River or Ashland are now the largest employers for 50 miles. Details Herman’s $430 million in community investment and how “healthcare capital” props up Main Street economies.
The Doctor Will Text You Now
Profiles Essentia’s embedded tech — patient portals, nurse hotlines, “Virtual Visits on Demand.” Asks whether tech can rebuild trust in small-town medicine or just widen the gap between those online and those left out.
Un-Burdening the Healers
Probes clinician burnout and the quiet hope behind Herman’s claim that value-based care restores purpose. Pairs physician interviews with workforce data — the new rural exodus of nurses, the pipeline from St. Scholastica and Itasca CC.
Policy from the North: How Duluth Is Whispering in Congress’s Ear
A reporter’s take on Herman’s Washington moment. Charts how Duluth’s CEO is lobbying for permanent telehealth, ACO bonuses, and parity between Medicare Advantage and alternative payment models — small-town voices shaping national reform.
Howie writes from Duluth, where he’s been poking the city’s sacred cows since before half the current council learned to parallel park. He runs HowieHanson.com, a one-man newsroom blogger powered by caffeine, sarcasm, and an allergy to PR spin. Part columnist, part historian, part irritant, he still believes in telling the truth—even when it makes the room uncomfortable.